A bioengineered corneal tissue has been developed using collagen protein from pig’s skin. Porcine dermal collagen was chemically and photochemically bioengineered into an implantable tissue mimicking the human corneal extracellular matrix. The implant has restored vision to people with advanced keratoconus.
An estimated 12.7 million people globally suffer blindness due to corneal disease. A transplanted cornea from a human donor is the only way of regaining vision for those patients. However, owing to a severe shortage of donor tissue and poor access to tissue banking infrastructure, only 1 in 70 patients who need corneal transplantation receive it. A solution to this problem is a bioengineered cornea.
Making the bioengineered corneal tissue
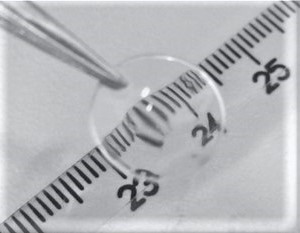
Researchers of LinkoCare Life Sciences AB, Linköping, Sweden used purified type I porcine collagen from pig’s skin to construct the “artificial cornea”. They engineered this collagen into an implantable tissue by chemically and photochemically creating collagen–collagen bonds (crosslinks) to strengthen the implant while maintaining high transparency.
At the same time, in collaboration with Linköping University, Linköping, Sweden, the researchers developed a minimally invasive technique to insert the implant within the existing cornea rather than replacing it. This surgical implantation technique was validated in a pig model using simple tools and in a single procedure, to avoid the need for suturing or long-term immunosuppression.
Clinical trial of the bioengineered corneal tissue
The researchers obtained approvals to conduct the first pilot study in India and Iran. Packaged implants and technical details of surgical implantation were transferred to the participating centers, where surgeons treated 20 individuals with advanced keratoconus on the waiting list for a corneal transplant, 14 of whom were legally blind.
Surgeons found the implants simple to insert, and operations were completed without complications, with only a short 8-week period of postoperative immunosuppressant medication. Postoperatively, corneas were transparent and stable, while the corneal thickness and curvature reverted to a pre-disease state. After 2 years of follow-up without adverse events, no patients were blind anymore, and vision in the entire group had improved to an equivalent degree as with standard transplantation with donor tissue. Three individuals in India who initially were blind achieved 20/20 vision.
The implications
This work demonstrates the possibility of manufacturing, storing (for up to 2 years before use) and distributing the implantable bioengineered tissue to regions with a high burden of corneal blindness. The proposed surgery is less invasive than traditional transplantation. Given the global shortage of donated corneas; the barriers to procuring, pathogen testing and storing donor tissue in certified tissue banks (where it needs to be used or discarded within 2 weeks); and the required long-term (at least 1 year) immunosuppression to avoid foreign tissue rejection, the proposed bioengineered alternative would be attractive, especially in resource-limited areas.
Still, longer-term clinical results and larger controlled trials for definitive evaluation of safety and efficacy are required before wider deployment of this technology.
References:
Lagali, N. and Rafat, M. Accessible bioengineered corneal tissue to address a blinding disease globally. Nat Biotechnol (2022). https://doi.org/10.1038/s41587-022-01409-9
Rafat, M., Jabbarvand, M., Sharma, N. et al. Bioengineered corneal tissue for minimally invasive vision restoration in advanced keratoconus in two clinical cohorts. Nat Biotechnol (2022). https://doi.org/10.1038/s41587-022-01408-w
See also:
First Pig to Human Heart Transplant
First Pig Heart Transplant: Recipient Died